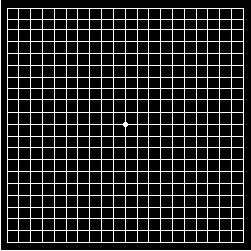
Amsler Grid Looks Like Graph Paper
Are you over age 55? Have you noticed a gradual, painless distortion or loss of central vision? Perhaps you have been diagnosed with Age-Related Macular Degeneration (ARMD).
As part of the management strategy for this condition, your eye doctor may have given you an Amsler Grid to take home with you. Amsler Grid looks like graph paper. It is a tool eye doctors may use to have you monitor any visual changes in your central vision at home. Since ARMD affects central vision, your eye doctor may give you an Amsler Grid in order for you to detect any loss of central vision quickly.
The grid is on a card and usually consists of white lines on a black background although you may be given one with black lines on a white background. The test is typically done at 13 to 14 inches, one eye at a time.
You will be instructed to look at the center dot, while being aware of the entire chart. As you look at the center dot, you will observe, without moving your eye, if you are able to see the four corners of the card as well as the four sides.
You will then be instructed to continue looking at the center dot. As you look at the center dot, you will note if there are any missing lines, wavy lines or missing boxes. If you notice any of these changes, you are to draw to the best of your ability the location and size of the abnormal area.
Is the Amsler Grid a good option?
The main advantage of the Grid is that it is cost effective and can be performed almost anywhere. The Grid has been the traditional method used to help patients self-monitor any central vision loss at home.
While it is true that if your eye doctor teaches you to monitor your sight at home this will help increase the chances of saving your vision, The Grid has its limitations:
- Amsler Grid demonstrates low sensitivity (about 29%). This means it will help you pick up new vision loss less than a third of the time.
- Amsler Grid testing relies on your compliance and your performance accuracy in doing the test.
- Amsler Grid cannot always compensate for the brain’s inherent ability to correct for visual impairment. Since the brain “knows” what the Amsler Grid should look like, it may fill in the blanks that the affected eye did not capture, yielding a false negative result; i.e., missing the vision loss altogether.
Numerous studies have cited these limitations of the Grid:
- Fixation issues (not looking only at the center dot during the test)
- Cortical
completion (which refers to the brain filling in missing information
not captured by the affected eye)
- Visual crowding
- By the time the Grid reveals metamorphopsia (which is marked by waviness of the lines of the grid and occurs when fluid is under the Macula); your condition may have already progressed significantly.
The image shows metamorphopsia (wavy lines indicative of fluid under the Macula) and scotoma (blind spot)
- The Grid is an especially challenging test because it requires that you delineate, on the chart, the perception of your vision defects, while fixating elsewhere. When compared with a gold standard micro-Visual Field test, the Amsler Grid fails to detect approximately half of the scotomas (blind spots) that are present.
What alternatives are there to Amsler Grid?
To address some of the limitations associated with the Grid testing, the Foresee Preferential Hyperacuity Perimeter (PHP) was designed specifically to monitor Dry ARMD patients for the early development of CNVMs.
The Foresee PHP is an FDA-approved device that employs the visual phenomenon of hyperacuity (or Vernier acuity). Hyperacuity is the ability to detect small differences in the relative location of visual stimuli.
The short test presents you with dot-deviation signals that include a misalignment, or artificial distortion, that you must identify. If your condition is advancing, you may identify a pathological distortion that is not actually present, rather than the test’s artificial distortion.
The Foresee PHP demonstrates 82% sensitivity as well as 88% specificity. Thus, in the majority of patients not only will this test be successful at identifying those with central vision loss, but it will be successful at identifying normal individuals as normal.
The Foresee PHP helps to show when you begin to exhibit retinal or RPE elevation. As ARMD progresses, drusen may cause retinal pigment epithelium elevation. This elevation subsequently creates pathological changes that can make straight lines appear distorted.
The Foresee PHP then generates a report, which indicates whether conversion from Dry to Wet ARMD is suspected. Your test results are compared with results from an ARMD normative database, which provides a comprehensive analysis.
Normative database has data that characterize what is usual in a defined population at a specific point or period of time. The Foresee PHP is in many cases able to identify CNVMs in patients who have no symptoms.
Your eye doctor may recommend that you take the test quarterly or more often if you demonstrate a high risk for conversion to Wet ARMD.
Another useful addition to the battery of tests used to monitor progression of ARMD is the Optical Coherence Tomography (OCT) test. While the Foresee PHP is a functional test that monitors your hyperacuity, the OCT provides an image of the retina that measures retinal thickness and reveals the presence of fluid.
Utilizing the ability of the OCT to measure changes in retinal thickness can help pinpoint the location of a change or pathology over time and help identify drusen that are growing in the RPE. Also, this instrument’s imaging capabilities can also confirm the presence of retinal bleeding caused by Wet ARMD.