What is Idiopathic Facial Nerve Paralysis (IFNP)? What is Bells Palsy?
Idiopathic Facial Nerve Paralysis (IFNP) or Bells Palsy is the most commonly encountered cranial neuropathy and it involves the seventh cranial nerve (i.e., facial nerve). The seventh cranial nerve is a mixed nerve that carries both motor and sensory impulses.
The facial nerve carries motor impulses for facial expressions and carries motor impulses to tear and salivary glands. Sensory fibers carry impulses from taste receptors on the anterior tongue. Bells Palsy is the most common type of acquired facial weakness.
What are the signs and symptoms of Bells Palsy?
Bells Palsy can be described by:
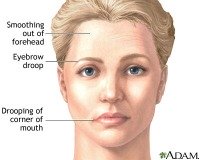
- Spontaneous onset of unilateral weakness of upper and lower muscles of one side of the face. The upper and lower eyelids, cheek, and the corner of the mouth show abnormal relaxation.
- Approximately 60% of patients have a preceding viral illness.
- Facial muscles pull to the opposite side on smiling
- Saliva and food may collect on the paralyzed side
- On attempting to close the eye the eyeball may be diverted upward and inward (Bells phenomenon)
- There may be decreased tearing in the affected eye. Rapid recognition of this symptom is important because these patients require artificial tears to lubricate the cornea and may need to have the eye taped shut to prevent drying and infection.
- Visual problems as a consequence of loss of the blink response and widening of the eye openings increase the potential for corneal exposure. The lower lid can turn out abnormally (ectropion) and further worsen the corneal exposure.
- This limited corneal protection can ultimately lead to corneal dryness, ulceration, and blindness if intervention is delayed.
Another secondary visual complication is that the upper lid sags over the eye (this is referred to as ptosis), leading to obstruction of the superior visual field.
- There may be a decrease in salivation and impaired taste in the anterior two-thirds of the tongue.
- Individuals afflicted deal with psychosocial disabilities that accompany the loss of facial nerve function.
- Increased sensitivity to heat, cold, and wind adds to the reduced quality of daily living.
Associated complaints with Bells Palsy in decreasing order of frequency include:
- Numbness or pain in front or behind the ear
- Alterations in taste
- Hyperacusis (abnormally acute hearing)
- Facial numbness ipsilateral (on the same side) to the side of weakness and decreased tearing in the affected eye
Other less common causes of facial paralysis must be considered before making the diagnosis of Bells Palsy. Associated conditions include:
- Diabetes Mellitus
- Hypertension
- Human Immunodeficiency Virus infection
- Lyme Disease
- Ramsay Hunt Syndrome (facial palsy with zoster oticus caused by varicella zoster virus)
- Sarcoidosis
- Sjogren’s syndrome
- Parotid nerve tumors
- Eclampsia
- Amyloidosis
- Peripheral facial nerve palsy has also been reported in recipients of inactivated intranasal influenza vaccine.
The herpes zoster virus is the most common confirmed infective cause for facial nerve paralysis resulting in the Ramsay Hunt Syndrome. Zoster vesicles erupt in the ear, external auditory canal, tongue, and hard palate. Often these patients experience ear and facial pain before the paralysis occurs.
Zoster patients portray a high incidence of complete paralysis. In comparison to Bell’s Palsy, patients with Ramsay Hunt Syndrome are less likely to recover completely and have a more severe painful paralysis associated with the ear symptoms. A little over half of these patients have a poor recovery.
Bell’s Palsy is managed in stages.
Stage 1
Early stages of management aim to speed recovery and limit corneal exposure and restore the blink response. The lower third of the cornea is often affected. Intensive lubrication is most commonly used in the early phases. Lubrication may be used in the form of preservative-free tear drops during the day and a more viscous ointment overnight. Taping of the eyelids at night prevents exposure and trauma while sleeping.
Stage 2: Medical
- Botulinum Toxin injection provides a good means of temporarily paralyzing the upper lid muscle (levator palpebrae superioris) and thus protect the cornea with eyelid closure.
- The use of steroids and oral acyclovir (an antiviral drug). The literature available regarding patients with incomplete paralysis points to no treatment as the best course of action as the majority recovers spontaneously. With initial complete paralysis, recovery is less predictable. Using steroids and oral acyclovir remains controversial. Because varicella zoster reactivation usually has a poorer prognosis than Bell’s Palsy, administration of acyclovir within 3 days of onset of facial paralysis may result in a high rate of recovery of the facial nerve as substantiated in a handful of studies. It has been recommended in the literature to treat all idiopathic (those with unknown cause) cases of Bell’s Palsy with acyclovir, as zoster may be causative even if not present with a vesicular rash.
Stage 3: Surgical
Surgical procedures are used less frequently in modern times to ensure adequate protection of the cornea during the acute phase. Tarsorrhaphy (sewing of the upper and lower lids together in order to close the eye) has been criticized for being cosmetically poor, often ineffective and for creating loss of peripheral vision. However, in patients in whom medical therapy is difficult and lacrimal gland function is lost, tarsorrhaphy remains an important treatment option. Other surgical procedures include resection of the upper eyelid muscle and upper lid weighting.
In a nutshell, the best treatment for these patients is multidisciplinary. Facial nerve paralysis spans across all races and ages. It occurs most commonly in the 15- to 45- year-old age group and represents social and psychological stigma.
The cause in Idiopathic Facial Nerve Paralysis (IFNP) remains uncertain. Your eye doctor will have a central role in the acute phase in protecting the cornea
Return From Bells Palsy to Eye Problems