|
Diabetic Retinopathy
Are you experiencing decreased vision? Are you seeing floating spots in your field of vision, otherwise known as floaters? Are you diabetic or suspect that you are? You may be suffering from Diabetic Retinopathy (DR). In order to view the content, you must install the Adobe Flash Player. Please click here to get started.
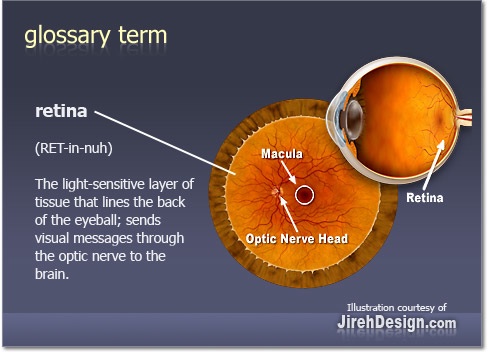
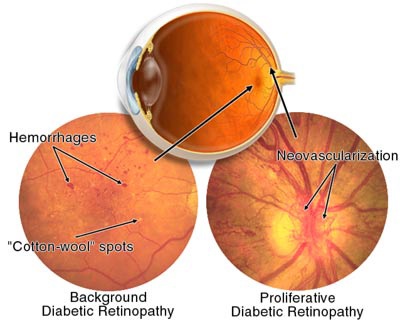
Diabetes is the seventh leading cause of death and the leading cause of blindness in adults aged 20 to 74 years, according to the American Diabetes Association (ADA). The incidence and severity of DR increases with the duration of diabetes and is likely to be worse if control of the diabetes is poor. Thus, the strongest risk factor for Diabetic Retinopathy is the disease’s duration, with 66% of those with diabetes for 15 or more years having the condition. Nearly 100% of people who have had diabetes for more than 30 years will show signs of DR. The other critical factor in prevention and slowing progression of DR is tight glycemic control and compliance with your diabetic regimen. Large fluctuations in glucose levels can cause damage to blood vessels of the retina. Early and less severe cases of DR, often referred to as Non-proliferative Diabetic Retinopathy are characterized by existing blood vessels in the retina becoming leaky and porous, causing blurred vision from the leaked fluid into the retina. The retina is the light-sensitive layer of tissue at the back of the inner eye. It acts like the film in a camera- images come through the eye’s cornea and lens and are focused on the retina. The retina then converts these images to electrical signals and sends them via the optic nerve to the brain. The retina has a rich blood supply, and when these vessels are affected by a disease such as DR, signs of bleeding and leaking of fluid will be noted by your eye doctor.
In the more advanced and severe type of DR, also known as Proliferative Diabetic Retinopathy, new blood vessels grow in the retina to compensate for the lower levels of oxygen available because the existing vessels are damaged, leaky and porous. The problem with these new blood vessels is that they are fragile and can hemorrhage causing loss of vision. Neovascularization shown below refers to new blood vessel growth.
How do you know if you are controlling your diabetes well?
Diabetic complications increase with increasing A1C levels. What if your diabetes control is poor?
You should be seeing your internist more frequently as well as your eye doctor if you have DR because you are more likely to have faster progression of the condition. Your physicians may be more aggressive about treatment decisions when you have borderline eye disease and your control of the disease is poor. What else can make your Diabetic Retinopathy progress faster?
The metabolic triad of diabetes, hypertension, and hypercholesterolemia can increase your risk of faster progression of Diabetic Retinopathy. Also, the acute problems that severe hypertension causes (such as kidney failure) can make progression of DR faster. Current recommendations for blood pressure control in diabetics suggest that the goal should be less than 130/80 mm Hg. Diabetic nephropathy (or kidney failure) can also be associated with retinopathy progression. You should have your kidney function tested if you have retinopathy. Other factors to consider: Additional factors that may play a role in retinopathy progression include: Besides monitoring for these health issues, what else can be done for Diabetic Retinopathy?
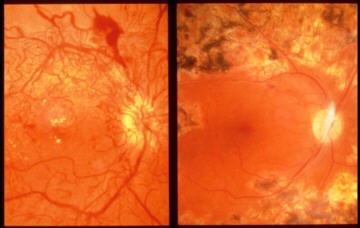
Laser surgery may be indicated to seal leaking vessels or destroy abnormal fragile vessels. Surgical treatment such as vitrectomy is used in cases of hemorrhage into the eye. Laser treatment may also be used to repair retinal detachment caused by hemorrhage and subsequent scarring. The image on the right shown below has been treated with laser.
|