|
Keratoconus:Is A Corneal Disease Marked by Corneal Thinning
Have you been noticing that each successive eye exam leaves you with a higher spectacle prescription? Has your eye doctor been telling you that your astigmatism is getting worse each visit? Has your eye doctor suggested that rigided contact lens may the best way to help you see well? You may have a condition of the cornea called Keratoconus. It is a corneal disease marked by corneal thinning (referred to as ectasia), which results in a bulging outward of the central cornea with subsequent corneal distortion and irregular astigmatism. The cornea is the outer, transparent, dome-like structure that covers the iris (the colored part of the eye), the pupil (the black hole in the middle of the iris), and the anterior chamber (the space between the iris and the back of the cornea filled with fluid). The cornea is part of the eye’s focusing system. 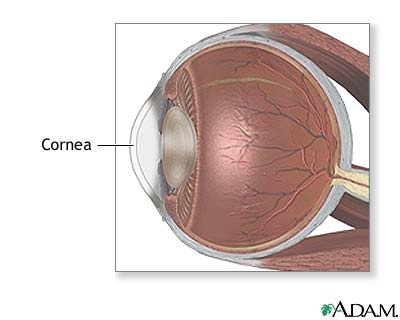
The cornea’s transparency and stability depends on its collagen. Collagen gives the cornea its strength, elasticity, and form. The collagen’s unique shape, arrangement, and spacing are essential in producing the cornea’s light-conducting transparency. The stability of the cornea is decreased due to increased pepsin digestion and fewer collagen cross-links. In essence, the collagen’s unique arrangement is altered, affecting the cornea’s shape. In order to view the content, you must install the Adobe Flash Player. Please click here to get started.
What are the major characteristics?
Cause is unknown, but there are some associations that can be made: Keratoconus is associated with several other disorders including: What can you expect as your Keratoconus progresses?
Because the shape of your cornea will be less stable and there will be a bulging outward of the cornea, you should expect that your irregular astigmatism should increase. As your prescription increases, your glasses will be less useful and there will come a time where the glasses will not give you adequate vision. Rigid contact lenses will provide superior vision to spectacles because the hard contact lens is placed on top of the irregular cornea, giving the eye a stable refracting surface. With the cornea’s progressive bulging, however, the rigid contact lenses will be less comfortable and stable in fit. Ultimately, when both spectacles and rigid contact lenses fail to give comfortable, good vision, a corneal transplant may be necessary. Are there any other options?
Both rigid contact lenses and corneal transplant do not treat the underlying cause of the corneal thinning, and therefore cannot stop the progression. There is a relatively new procedure called Corneal Collagen Cross-Linking (CXL), which is currently under investigation in the US to determine if it can slow, stabilize, or even possibly reverse the progression of corneal thinning in patients with Keratoconus. CXL is already being used in many centers worldwide as a first-line treatment for. CXL increases the rigidity of the cornea by inducing additional cross-links within or among collagen fibers using ultraviolet-A (UVA) light and riboflavin. As with many conditions, the earlier the patient is treated, the better the results. The CXL-USA Study Group is actively enrolling patients in a multicenter investigational study to gather data on the safety, efficacy, and optimal techniques for cross-linking. For more information about this study or for more information about Keratoconus, visit: Corneal Collagen Cross-Linking. |




